建議
18 歲以下第1型糖尿病童的血糖建議控制目標為空腹血糖 90-130 mg/dl,睡前血糖 90-150 mg/dl,HbA1c < 7.5%,並再次強調指標需個別化調整
Type 2 Diabetes Glucose Management Goals
Glycemic targets
美國內分泌臨床醫師協會AACE 建議可將A1C目標值設定在 6.5 以下.
美國糖尿病學會ADA則建議將一般成人A1C目標設定在 7.0 以下
(ADA也建議, 在選擇性的病患, 可將控制目標設為6.5以下例如沒有其他疾病, 預期還有很長的生命, 低血糖風險低, 容易達成目標)
糖化血色素控制目標, 需根據病患特性考量, 多數病患, 建議控制 A1C ≤7.0 %
老年人或有其他共病症的患者, 或預期壽命有限的患者, A1C 標準可上調.
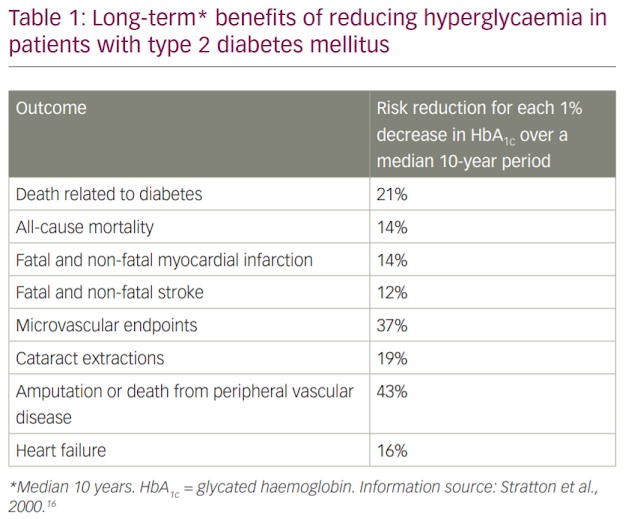
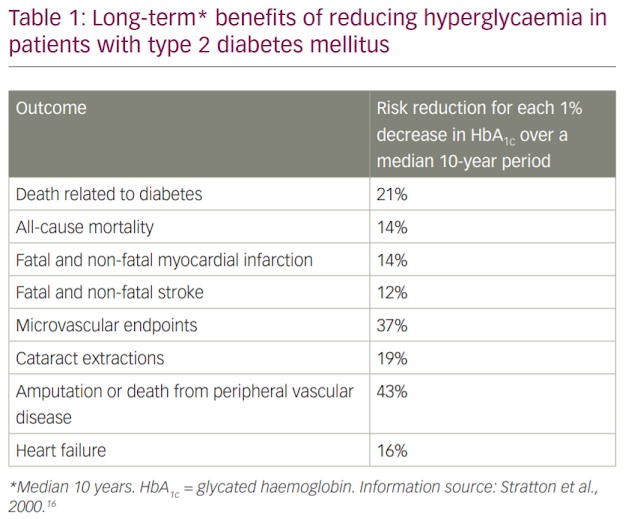
●Glycated hemoglobin (A1C) – Target A1C levels in patients with type 2 diabetes taking insulin should be tailored to the individual, balancing the reduction in microvascular complications (figure 1) with the risk of hypoglycemia and insulin-associated weight gain. A reasonable goal of therapy for most patients might be an A1C value ≤7.0 percent (using an assay aligned to the Diabetes Control and Complications Trial [DCCT] in which the upper limit of normal is 6.0 percent). The A1C goal should be set somewhat higher for older patients, patients with comorbidities, and those with a limited life expectancy. (See "Glycemic control and vascular complications in type 2 diabetes mellitus".)
空腹血糖, 健康人如果要讓A1C小於7, 空腹血糖值通常在 80-130 之間, 老年人如果有慢性腎病, 有低血糖風險, 這些病患的A1C目標值可調高, 空腹血糖標準也可以上調至 150.
●Fasting blood glucose (FBG) – In general, for healthy young and middle-aged adults to achieve an A1C goal ≤7.0 percent, an FBG of 80 to 130 mg/dL (4.4 to 7.2 mmol/L) is usually necessary, but slightly higher levels may suffice [2,3]. In older patients, those with chronic kidney disease, or those with other risk factors for hypoglycemia, in whom the A1C goal is set higher, a higher FBG target (eg, 150 mg/dL) may be used.
美國內分泌臨床醫師協會AACE 建議根據病患的年齡, 共病症, 低血糖風險等等因素來制訂A1C 目標值. 如果身體狀況良好, 可將A1C目標設定在 6.5 以下.
T2D Pharmacotherapy
In patients with T2D, achieving the glucose and A1C targets requires a nuanced approach that balances age, comorbidities, hypoglycemia risk, and many other factors described above (4). The AACE supports an A1C goal of ≤6.5% (48 mmol/mol) for most patients or >6.5% if the lower target cannot be achieved without adverse outcomes. Significant reductions in the risk or progression of nephropathy were seen in the ADVANCE (Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation) study, which targeted an A1C <6.5% in the intensive therapy group versus standard approaches. In ADVANCE, the starting A1C was 7.5% (58 mmol/mol), and rates of hypoglycemia were higher in the intensive therapy group (173). In the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial, intensive glycemic control significantly reduced the risk and/or progression of retinopathy, nephropathy, and neuropathy (174,175). However, in ACCORD, which involved older and middle-aged patients with long-standing T2D who were at high risk for or had established ASCVD and a baseline A1C >8.5% (69 mmol/mol), patients randomized to intensive glucose-lowering therapy (A1C target of <6.0% [42 mmol/mol]) had increased mortality (176). The excess mortality occurred only in patients whose A1C remained >7% (53 mmol/mol) despite intensive therapy, and this critical distinction is sometimes forgotten when the risk and benefits of intensive therapy are discussed. In the standard therapy group (A1C target 7 to 8% [53 to 64 mmol/mol]), mortality followed a U-shaped curve with increasing death rates at both low (<7%) and high (>8%) A1C levels (177). ACCORD showed that cardiovascular autonomic neuropathy may be another useful predictor of cardiovascular risk (178). A combination of cardiovascular autonomic neuropathy and symptoms of peripheral neuropathy increase the odds ratio to 4.55 for ASCVD and mortality (179). In the Veterans Affairs Diabetes Trial (VADT), which had a higher A1C target for intensively treated patients (1.5% lower than the standard treatment group), there were no between-group differences in ASCVD endpoints, cardiovascular death, or overall death during the 5.6-year study period (176,180). After approximately 10 years, however, VADT patients participating in an observational follow-up study were 17% less likely to have a major cardiovascular event if they received intensive therapy during the trial (P<.04; 8.6 fewer cardiovascular events per 1,000 person-years), while mortality risk remained the same between treatment groups
The hemoglobin A1C (A1C) target should be individualized based on numerous factors, such as age, life expectancy, comorbid conditions, duration of diabetes, risk of hypoglycemia or adverse consequences from hypoglycemia, patient motivation, and adherence. Glycemic control targets include fasting and postprandial glucose as determined by self-monitoring of blood glucose (SMBG). In recent years, continuous glucose monitoring (CGM) has become more available for people with T2D and has added a considerable degree of clarity for the patient's and clinician's understanding of the glycemic pattern.
An A1C level of ≤6.5% (48 mmol/mol) is considered optimal if it can be achieved in a safe and affordable manner, but higher targets may be appropriate for certain individuals and may change for a given individual over time.
Severe hypoglycemia occurs more frequently with intensive glycemic control in RCTs where insulin and/or sulfonylureas (SUs) are utilized (173,176,180,182,183). In ACCORD, severe hypoglycemia may have accounted for a substantial portion of excess mortality among patients receiving intensive therapy, although the hazard ratio for hypoglycemia-associated deaths was higher in the standard treatment group (183).
Taken together, this evidence supports individualization of glycemic goals (see Comprehensive Type 2 Diabetes Management Algorithm—Glycemic Control Algorithm) (4). In adults with recent T2D onset and no clinically significant ASCVD, an A1C ≤6.5% (48 mmol/mol), if achieved without substantial hypoglycemia or other unacceptable consequences, may reduce the lifetime risk of micro- and macrovascular complications. A broader A1C range may be suitable for older patients and those at risk for hypoglycemia. A less stringent A1C >6.5% is appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced renal disease or macrovascular complications, extensive comorbid conditions, or long-standing T2D in which the A1C goal has been difficult to attain despite intensive efforts, so long as the patient remains free of polydipsia, polyuria, polyphagia, or other hyperglycemia-associated symptoms. Therefore, selection of glucose-lowering agents should consider a patient's therapeutic goal, age, and other factors that impose limitations on treatment, as well as the attributes and adverse effects of each regimen. Regardless of the treatment selected, patients must be followed regularly and closely to ensure that glycemic goals are met and maintained.
ADA關於A1C 的建議
A1C GOALS
For glycemic goals in older adults, please refer to Section 12 “Older Adults.” For glycemic goals in children, please refer to Section 13 “Children and Adolescents.” For glycemic goals in pregnant women, please refer to Section 14 “Management of Diabetes in Pregnancy.”
Recommendations
6.4 A reasonable A1C goal for many nonpregnant adults is <7% (53 mmol/mol). A
6.5 Providers might reasonably suggest more stringent A1C goals (such as <6.5% [48 mmol/mol]) for selected individual patients if this can be achieved without significant hypoglycemia or other adverse effects of treatment (i.e., polypharmacy). Appropriate patients might include those with short duration of diabetes, type 2 diabetes treated with lifestyle or metformin only, long life expectancy, or no significant cardiovascular disease. C
6.6 Less stringent A1C goals (such as <8% [64 mmol/mol]) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, extensive comorbid conditions, or long-standing diabetes in whom the goal is difficult to achieve despite diabetes self-management education, appropriate glucose monitoring, and effective doses of multiple glucose-lowering agents including insulin. B
6.7 Reassess glycemic targets over time based on the criteria in Fig. 6.1 or, in older adults, Table 12.1. E
However, on the basis of physician judgment and patient preferences, select patients, especially those with little comorbidity and long life expectancy, may benefit from adopting more intensive glycemic targets (e.g., A1C target <6.5% [48 mmol/mol]) if they can achieve it safely without hypoglycemia or significant therapeutic burden.
高血壓 高尿酸 慢性腎病 胰島素 https://2019medicinenote.blogspot.com/2019/12/blog-post_57.html . 糖尿病相關筆記~目錄 https://2019medicinenote.blogspot.com/2020/01/blog-post_4.html
高血壓 高尿酸 慢性腎病 胰島素 https://2019medicinenote.blogspot.com/2019/12/blog-post_57.html . 糖尿病相關筆記~目錄 https://2019medicinenote.blogspot.com/2020/01/blog-post_4.html
2019年12月28日 星期六
第二代基礎胰島素類似物效益與安全性比較-回顧現有的資料
2017-11-17 Comparative Efficacy and Safety of Second-generation Basal Insulin
Analogues – a Review of Emerging Comparative Data
第二代胰島素類似物~ 迄今為止的故事
與第一代基礎胰島素類似物 (Gla-100)比較, 對於T2DM, 第二代基礎胰島素類似物 Gla-300 及 IDeg-100 (IDeg-100 或簡稱 IDeg) 有較佳的藥物動力學及藥效學, 能更穩定的控制血糖 (一天之間變動較小), 低血糖機率也降低, 一天僅需注射一次, 注射時間也很彈性
第二代基礎胰島素類似物優於第一代基礎胰島素類似物, 但第二代基礎胰島素之間的互相比較, 資料不多.
Second-generation basal insulin analogues – the story so far
Compared with first-generation basal insulin analogues, second generation treatments (insulin largine 300 U/mL [Gla-300] and insulin degludec [IDeg]) have demonstrated improved pharmacokinetic (PK) and pharmacodynamic (PD) profiles that provide greater glucose stability (less intra-day variation), together with a lower risk of hypoglycaemia, in patients with type 2 diabetes mellitus (T2DM). As a result, clinicians now have insulin treatment options that provide glycaemic control with the benefit of a stable, ultra-long duration of action that allows once-daily administration with flexibility in daily injection time. However, while the available evidence demonstrates that Gla-300 and IDeg provide similar clinical benefits to first-generation basal insulin analogues (albeit via different mechanisms of action), no direct comparison between the second-generation basal insulin analogues has been presented to date.
第十一屆先進糖尿病技術與治療共識會, 有三篇第二代基礎胰島素類似物的研究
DELIVER-D study
LIGHTNING
the BRIGHT study 是第一篇關於第二代基礎胰島素類似物正面交鋒 (head to head)隨機控制研究(RCT)
Emerging data from the 11th International Conference on Advanced Technologies & Treatments for Diabetes (ATTD)
Data from three studies of second-generation basal insulin analogues were presented at ATTD (Vienna, Austria) in February 2018. Real-world evidence from the DELIVER-D study was validated by a second realworld study, LIGHTNING, which used a similar methodology applied to a larger source dataset of electronic medical records. In addition to the real-world studies, the BRIGHT study provides the first randomised controlled trial (RCT) evidence from a head-to-head comparison of second-generation basal insulin analogues. The most recent data from each of these three studies (DELIVER-D, LIGHTNING, BRIGHT) were presented at the ATTD 2018 meeting and are reviewed here.
當病患的治療從第一代基礎胰島素類似物轉換成第二代基礎胰島素類似物
第二代胰島素類似物 (Gla-300 in EDITION, IDeg in BEGIN) 相較於第一代基礎胰島素類似物 (Gla-100) , 治療效果穩定且安全性提高, 但這些研究中, 低血糖病患常常被排除掉, 此外, 也沒有關於 Gla-300 與 IDeg 兩者的比較 Assessing comparative real-world findings in patients switching from first- to second generation basal insulin analogues DELIVER-D
Previously published data from the EDITION and BEGIN clinical trials and subsequent meta-analyses have demonstrated consistent efficacy and improved safety profiles for second-generation basal insulin analogues (Gla-300 in EDITION and IDeg in BEGIN), compared with insulin glargine 100 U/mL (Gla-100). However, the extent to which these findings from strictly controlled RCT settings are applicable to real-life practice has yet to be examined. In these initial trials, patients with hypoglycaemia were often excluded. In addition, no direct comparisons between Gla-300 and IDeg have been presented to date.
DELIVER-D 研究是回溯性觀察性研究, 在美國使用第一代基礎胰島素類似物的病患, 換成第二代基礎胰島素類似物後, 根據電子醫療紀錄評估安全性與效益, 調查第二代基礎胰島素類似物正面交鋒的差異, 這篇研究資料來自 PHIED, 涵蓋 39 個美國健康照護整合網絡, 收集T2DM成人病患從 Gla-100 換成 Gla-300 or IDeg(IDeg-100 or IDeg-200, 台灣好像沒有進 IDeg-200), 病患在過去六個月內至少曾處方一次 Gla-100, 且在此期間沒有使用其他基礎胰島素 DELIVER-D was a retrospective, observational study assessing safety and efficacy outcomes from electronic medical records in patients in the US switching from first-generation Gla-100 to either Gla-300 or IDeg. Head-to-head differences between the two second-generation basal insulin analogues were investigated.8 DELIVER-D assessed data from the Predictive Health Intelligence Environment database, which covers 39 integrated US healthcare networks. Data were gathered for adult patients with T2DM who were switched from Gla-100 to either Gla-300, IDeg 100 U/mL or IDeg 200 U/mL (index date: first prescription date during the period 1st March 2015 to 31st December 2016) and who had at least one Gla-100 prescription within 6 months before the index date (baseline period), but who had not received any other basal insulin prescriptions during this period.
病患需要有至少先前12個月的電子醫療紀錄才能被收錄, 且收案後需有 6 個月以上的記錄, 且在六個月的基準期至少有一次A1C測量數據, 根據傾向分數隨機配對成 Gla-300 或 IDeg.
在傾向分數配對後, Gla-300 與 IDeg 兩組, 先前12個月的人口統計與基礎值相似.
評估病患在6個月追蹤期間, 根據先前基礎值低血糖事件率, 調整後的低血糖 (血糖<70)發生率及事件發生率(每人每年)
In order to be included in the study, patients were required to have electronic medical records for at least 12 months prior to, and at least 6 months following the index date, and to have had at least one glycated haemoglobin (HbA1c) measurement during the 6-month baseline period.8 Patients who switched from Gla-100 to Gla-300 or IDeg were matched in a 1:1 ratio using a propensity score based on: baseline demographics (age, gender, race, insurance type, geographic region); their clinical characteristics 12 months prior to the index date (body mass index, Charlson comorbidity index score, prevalence of comorbidities, concomitant medication use); and their clinical characteristics within the 6-month baseline period (HbA1c, hypoglycaemia incidence, utilisation of all-cause health care). After propensity score matching, the Gla300 (n=810) and IDeg (n=810) cohorts were comparable in terms of demographics and baseline characteristics.8 The DELIVER-D study included endpoints in both the full matched cohorts and in a subgroup of patients with HbA1c measurements at both the 6-month baseline and during 3–6 months of follow-up. In the matched cohorts, both the incidence of hypoglycaemia (identified by International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]/ International Classification of Diseases, 10th Revision, Clinical Modification [ICD-10-CM]) code and/or plasma glucose level ≤70 mg/dL [3.9 mmol/L]) and the event rate (events per patient per year [PPPY], adjusted for baseline hypoglycaemia event) during the 6-month follow-up period were assessed.
在subgroup中, 檢視的治療終點是 A1C 下降值, 及達到目標值A1C 的病患比例.
In the subgroup, the endpoints examined were HbA1c reduction from baseline (closest to index date) at follow-up (latest available value during the follow-up period), and the proportion of patients attaining target HbA1c.
Gla-300 與IDeg 降低A1C的療效相似 (A1C 降低 0.49% VS 0.48%), 達成目標血糖的病患比例相近 (A1C <7.0% 12.9% VS 15.9%) (A1C<8.0% 44.2% VS 44.6%)
在更換藥物期間, 病患低血糖機率降低, 根據基礎值調整後的低血糖發生率, 兩組沒有明顯差異
兩種第二代基礎胰島素類似物, 低血糖事件減少的機率相近, 降低低血糖急診就診機率與低血糖住院率也相近,
以上資料顯示, 兩種第二代基礎胰島素類似物療效與安全性都有改善
Both Gla-300 and IDeg provided similar clinically meaningful decreases in HbA1c following switching (0.49% and 0.48% reductions in HbA1c, respectively) and enabled similar proportions of patients to achieve the target HbA1c of either <7.0% or <8.0% (12.9% versus 15.9% and 44.2% versus 44.6%, respectively). Following switching, patients on the second generation treatments experienced a lower incidence of hypoglycaemia versus baseline (Gla-300: 16.5 to 11.9%; IDeg: 15.4 to 12.7%); there was no significant difference between Gla-300 and IDeg when adjusted for baseline hypoglycaemia incidence (Figure 1). Both second-generation treatments provided similar reductions in the average number of hypoglycaemia events per year (least squares mean [LSM] difference in event rate -0.01 events/PPPY, 95% confidence interval [CI] [-0.18, 0.15], p=0.88) and the rate of emergency visits or hospitalisations for hypoglycaemia (LSM difference in event rate -0.01 events/PPPY, 95% CI [-0.12, 0.09], p=0.82). Until RCT data are available to support head-to-head comparisons, these data provide valuable insights into real-world outcomes and demonstrate the improved efficacy and safety profiles of modern second-generation basal insulin analogues in routine clinical practice.
LIGHTNING 研究, 評估T2DM 從 Gla-100 或 IDet, 轉換成 Gla-300 or IDeg 的效益與安全性,
Humedica electronic health records- 來自50個美國的健康照護系統, 700 間醫院, 7000 位醫師, 500萬個T2DM病患
資料包括有 77萬9813名使用基礎胰島素類似物治療的患者, 13萬155筆使用基礎胰島素類似物治療符合收案條件, 排除可能是 T1DM 病患, 排除研究期間更換使用基礎胰島素十次以上病患,
The LIGHTNING study assessed real-world efficacy and safety outcomes in patients with T2DM switching to first- (Gla-100 or insulin detemir [IDet]) or second-generation (Gla-300 or IDeg) basal insulin analogues. Preliminary results of an analysis of Humedica electronic health records – a database capturing data from over 5 million people with diabetes across more than 50 US healthcare systems, 700 hospitals and 7,000 clinics – from 1st April 2015 to 31st December 2016 – are presented here.9 The dataset included 779,813 people with T2DM receiving basal insulin analogues. A total of 130,155 basal insulin analogue treatments complied with the study inclusion criteria (Figure 2), representing patients either initiating a new basal insulin or switching between basal insulins. Patients were excluded from the study if they had a likely predominant diagnosis of type 1 diabetes, or if they had more than 10 basal insulin switches within the study window (as such cases
would likely represent unusual clinical behaviour).9
使用 patient treatment 做為一個研究單位. 僅計算在每個 patient treatment 治療期間的低血糖事件,
Data presented here focus only on findings in patients switching between basal insulin treatment options. The study approached its assessment using an analysis unit of ‘patient treatment’ – the period of time between treatment index (basal insulin initiation or switching event) and treatment end – and only counted on-treatment hypoglycaemic events during each patient treatment unit. Propensity score matching was used to match cohorts for potentially confounding characteristics, allowing for between treatment comparison.
關鍵結果包括嚴重低血糖發生率, A1C 與基礎值的變化, 嚴重低血糖定義為血糖 < 70, 需要住院或急診治療, A1C 變化則是計算基礎值與追蹤 76-180 天的變化.
Key outcomes included the incidence of severe hypoglycaemia and HbA1c change from baseline in a subgroup of patients with HbA1c measurements in both time windows. Severe hypoglycaemia was defined as any hypoglycaemic event (ICD-9 or ICD-10 identified or plasma glucose ≤70 mg/dL [3.9 mmol/L]) related to an inpatient or emergency department encounter. HbA1c change was assessed as change from baseline to 76–180 days’ follow-up.9
不管先前使用哪一種第一代基礎胰島素類似物, 使用 Gla-300 的病患, 嚴重低血糖機率顯著降低
Switching from any basal insulin, patients who switched to Gla-300 had a significantly lower incidence of severe hypoglycaemia versus patients switched to the first-generation basal insulin analogues Gla-100 and IDet (p=0.009 and p=0.002, respectively).
第二代基礎胰島素 IDeg 與 Gla-300 比較, 兩組嚴重低血糖降低的機率相似
總體來說, 換成 Gla-100, IDet, Gla-300, A1C 降低幅度相似, 而第二代基礎胰島素之間的結果也相似.
不管病患之前使用哪一種基礎胰島素, 換成 Gla-100, Gla-300, IDet, IDeg, 在這項大型觀察性研究報告也支持 DELIVER-D 的研究結果,
第二代基礎胰島素類似物, 相較於第一代基礎胰島素, 改善的效益與安全性相近.
第二代基礎胰島素治療, 降低嚴重低血糖的機率也相近.
In the direct comparison between second-generation basal insulins, IDeg and Gla-300 provided similar reductions (p=0.370) in the rate of severe hypoglycaemia (Figure 3).9 Overall, results of the analysis showed that there was a similar reduction in HbA1c for patients switching to Gla-100, IDet and Gla-300, and similarly there was no significant difference between the second-generation treatments (Gla-300 and IDeg; p=0.591; Figure 4).9 Findings from this large, observational study of patients switching from any basal insulin to Gla-100, Gla-300, IDet or IDeg support the conclusions of DELIVER-D: that in real-world populations, second-generation basal insulin analogues provide similar efficacy and improved safety profiles versus first-generation agents. Both second-generation treatments (Gla-300 and IDeg) provided similar reductions in the rate of severe hypoglycaemia during a 6-month follow-up.
Analogues – a Review of Emerging Comparative Data
第二代胰島素類似物~ 迄今為止的故事
與第一代基礎胰島素類似物 (Gla-100)比較, 對於T2DM, 第二代基礎胰島素類似物 Gla-300 及 IDeg-100 (IDeg-100 或簡稱 IDeg) 有較佳的藥物動力學及藥效學, 能更穩定的控制血糖 (一天之間變動較小), 低血糖機率也降低, 一天僅需注射一次, 注射時間也很彈性
第二代基礎胰島素類似物優於第一代基礎胰島素類似物, 但第二代基礎胰島素之間的互相比較, 資料不多.
Second-generation basal insulin analogues – the story so far
Compared with first-generation basal insulin analogues, second generation treatments (insulin largine 300 U/mL [Gla-300] and insulin degludec [IDeg]) have demonstrated improved pharmacokinetic (PK) and pharmacodynamic (PD) profiles that provide greater glucose stability (less intra-day variation), together with a lower risk of hypoglycaemia, in patients with type 2 diabetes mellitus (T2DM). As a result, clinicians now have insulin treatment options that provide glycaemic control with the benefit of a stable, ultra-long duration of action that allows once-daily administration with flexibility in daily injection time. However, while the available evidence demonstrates that Gla-300 and IDeg provide similar clinical benefits to first-generation basal insulin analogues (albeit via different mechanisms of action), no direct comparison between the second-generation basal insulin analogues has been presented to date.
第十一屆先進糖尿病技術與治療共識會, 有三篇第二代基礎胰島素類似物的研究
DELIVER-D study
LIGHTNING
the BRIGHT study 是第一篇關於第二代基礎胰島素類似物正面交鋒 (head to head)隨機控制研究(RCT)
Emerging data from the 11th International Conference on Advanced Technologies & Treatments for Diabetes (ATTD)
Data from three studies of second-generation basal insulin analogues were presented at ATTD (Vienna, Austria) in February 2018. Real-world evidence from the DELIVER-D study was validated by a second realworld study, LIGHTNING, which used a similar methodology applied to a larger source dataset of electronic medical records. In addition to the real-world studies, the BRIGHT study provides the first randomised controlled trial (RCT) evidence from a head-to-head comparison of second-generation basal insulin analogues. The most recent data from each of these three studies (DELIVER-D, LIGHTNING, BRIGHT) were presented at the ATTD 2018 meeting and are reviewed here.
當病患的治療從第一代基礎胰島素類似物轉換成第二代基礎胰島素類似物
第二代胰島素類似物 (Gla-300 in EDITION, IDeg in BEGIN) 相較於第一代基礎胰島素類似物 (Gla-100) , 治療效果穩定且安全性提高, 但這些研究中, 低血糖病患常常被排除掉, 此外, 也沒有關於 Gla-300 與 IDeg 兩者的比較 Assessing comparative real-world findings in patients switching from first- to second generation basal insulin analogues DELIVER-D
Previously published data from the EDITION and BEGIN clinical trials and subsequent meta-analyses have demonstrated consistent efficacy and improved safety profiles for second-generation basal insulin analogues (Gla-300 in EDITION and IDeg in BEGIN), compared with insulin glargine 100 U/mL (Gla-100). However, the extent to which these findings from strictly controlled RCT settings are applicable to real-life practice has yet to be examined. In these initial trials, patients with hypoglycaemia were often excluded. In addition, no direct comparisons between Gla-300 and IDeg have been presented to date.
DELIVER-D 研究是回溯性觀察性研究, 在美國使用第一代基礎胰島素類似物的病患, 換成第二代基礎胰島素類似物後, 根據電子醫療紀錄評估安全性與效益, 調查第二代基礎胰島素類似物正面交鋒的差異, 這篇研究資料來自 PHIED, 涵蓋 39 個美國健康照護整合網絡, 收集T2DM成人病患從 Gla-100 換成 Gla-300 or IDeg(IDeg-100 or IDeg-200, 台灣好像沒有進 IDeg-200), 病患在過去六個月內至少曾處方一次 Gla-100, 且在此期間沒有使用其他基礎胰島素 DELIVER-D was a retrospective, observational study assessing safety and efficacy outcomes from electronic medical records in patients in the US switching from first-generation Gla-100 to either Gla-300 or IDeg. Head-to-head differences between the two second-generation basal insulin analogues were investigated.8 DELIVER-D assessed data from the Predictive Health Intelligence Environment database, which covers 39 integrated US healthcare networks. Data were gathered for adult patients with T2DM who were switched from Gla-100 to either Gla-300, IDeg 100 U/mL or IDeg 200 U/mL (index date: first prescription date during the period 1st March 2015 to 31st December 2016) and who had at least one Gla-100 prescription within 6 months before the index date (baseline period), but who had not received any other basal insulin prescriptions during this period.
病患需要有至少先前12個月的電子醫療紀錄才能被收錄, 且收案後需有 6 個月以上的記錄, 且在六個月的基準期至少有一次A1C測量數據, 根據傾向分數隨機配對成 Gla-300 或 IDeg.
在傾向分數配對後, Gla-300 與 IDeg 兩組, 先前12個月的人口統計與基礎值相似.
評估病患在6個月追蹤期間, 根據先前基礎值低血糖事件率, 調整後的低血糖 (血糖<70)發生率及事件發生率(每人每年)
In order to be included in the study, patients were required to have electronic medical records for at least 12 months prior to, and at least 6 months following the index date, and to have had at least one glycated haemoglobin (HbA1c) measurement during the 6-month baseline period.8 Patients who switched from Gla-100 to Gla-300 or IDeg were matched in a 1:1 ratio using a propensity score based on: baseline demographics (age, gender, race, insurance type, geographic region); their clinical characteristics 12 months prior to the index date (body mass index, Charlson comorbidity index score, prevalence of comorbidities, concomitant medication use); and their clinical characteristics within the 6-month baseline period (HbA1c, hypoglycaemia incidence, utilisation of all-cause health care). After propensity score matching, the Gla300 (n=810) and IDeg (n=810) cohorts were comparable in terms of demographics and baseline characteristics.8 The DELIVER-D study included endpoints in both the full matched cohorts and in a subgroup of patients with HbA1c measurements at both the 6-month baseline and during 3–6 months of follow-up. In the matched cohorts, both the incidence of hypoglycaemia (identified by International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM]/ International Classification of Diseases, 10th Revision, Clinical Modification [ICD-10-CM]) code and/or plasma glucose level ≤70 mg/dL [3.9 mmol/L]) and the event rate (events per patient per year [PPPY], adjusted for baseline hypoglycaemia event) during the 6-month follow-up period were assessed.
在subgroup中, 檢視的治療終點是 A1C 下降值, 及達到目標值A1C 的病患比例.
In the subgroup, the endpoints examined were HbA1c reduction from baseline (closest to index date) at follow-up (latest available value during the follow-up period), and the proportion of patients attaining target HbA1c.
Gla-300 與IDeg 降低A1C的療效相似 (A1C 降低 0.49% VS 0.48%), 達成目標血糖的病患比例相近 (A1C <7.0% 12.9% VS 15.9%) (A1C<8.0% 44.2% VS 44.6%)
在更換藥物期間, 病患低血糖機率降低, 根據基礎值調整後的低血糖發生率, 兩組沒有明顯差異
兩種第二代基礎胰島素類似物, 低血糖事件減少的機率相近, 降低低血糖急診就診機率與低血糖住院率也相近,
以上資料顯示, 兩種第二代基礎胰島素類似物療效與安全性都有改善
Both Gla-300 and IDeg provided similar clinically meaningful decreases in HbA1c following switching (0.49% and 0.48% reductions in HbA1c, respectively) and enabled similar proportions of patients to achieve the target HbA1c of either <7.0% or <8.0% (12.9% versus 15.9% and 44.2% versus 44.6%, respectively). Following switching, patients on the second generation treatments experienced a lower incidence of hypoglycaemia versus baseline (Gla-300: 16.5 to 11.9%; IDeg: 15.4 to 12.7%); there was no significant difference between Gla-300 and IDeg when adjusted for baseline hypoglycaemia incidence (Figure 1). Both second-generation treatments provided similar reductions in the average number of hypoglycaemia events per year (least squares mean [LSM] difference in event rate -0.01 events/PPPY, 95% confidence interval [CI] [-0.18, 0.15], p=0.88) and the rate of emergency visits or hospitalisations for hypoglycaemia (LSM difference in event rate -0.01 events/PPPY, 95% CI [-0.12, 0.09], p=0.82). Until RCT data are available to support head-to-head comparisons, these data provide valuable insights into real-world outcomes and demonstrate the improved efficacy and safety profiles of modern second-generation basal insulin analogues in routine clinical practice.
LIGHTNING 研究, 評估T2DM 從 Gla-100 或 IDet, 轉換成 Gla-300 or IDeg 的效益與安全性,
Humedica electronic health records- 來自50個美國的健康照護系統, 700 間醫院, 7000 位醫師, 500萬個T2DM病患
資料包括有 77萬9813名使用基礎胰島素類似物治療的患者, 13萬155筆使用基礎胰島素類似物治療符合收案條件, 排除可能是 T1DM 病患, 排除研究期間更換使用基礎胰島素十次以上病患,
would likely represent unusual clinical behaviour).9
使用 patient treatment 做為一個研究單位. 僅計算在每個 patient treatment 治療期間的低血糖事件,
Data presented here focus only on findings in patients switching between basal insulin treatment options. The study approached its assessment using an analysis unit of ‘patient treatment’ – the period of time between treatment index (basal insulin initiation or switching event) and treatment end – and only counted on-treatment hypoglycaemic events during each patient treatment unit. Propensity score matching was used to match cohorts for potentially confounding characteristics, allowing for between treatment comparison.
關鍵結果包括嚴重低血糖發生率, A1C 與基礎值的變化, 嚴重低血糖定義為血糖 < 70, 需要住院或急診治療, A1C 變化則是計算基礎值與追蹤 76-180 天的變化.
Key outcomes included the incidence of severe hypoglycaemia and HbA1c change from baseline in a subgroup of patients with HbA1c measurements in both time windows. Severe hypoglycaemia was defined as any hypoglycaemic event (ICD-9 or ICD-10 identified or plasma glucose ≤70 mg/dL [3.9 mmol/L]) related to an inpatient or emergency department encounter. HbA1c change was assessed as change from baseline to 76–180 days’ follow-up.9
不管先前使用哪一種第一代基礎胰島素類似物, 使用 Gla-300 的病患, 嚴重低血糖機率顯著降低
Switching from any basal insulin, patients who switched to Gla-300 had a significantly lower incidence of severe hypoglycaemia versus patients switched to the first-generation basal insulin analogues Gla-100 and IDet (p=0.009 and p=0.002, respectively).
第二代基礎胰島素 IDeg 與 Gla-300 比較, 兩組嚴重低血糖降低的機率相似
總體來說, 換成 Gla-100, IDet, Gla-300, A1C 降低幅度相似, 而第二代基礎胰島素之間的結果也相似.
不管病患之前使用哪一種基礎胰島素, 換成 Gla-100, Gla-300, IDet, IDeg, 在這項大型觀察性研究報告也支持 DELIVER-D 的研究結果,
第二代基礎胰島素類似物, 相較於第一代基礎胰島素, 改善的效益與安全性相近.
第二代基礎胰島素治療, 降低嚴重低血糖的機率也相近.
In the direct comparison between second-generation basal insulins, IDeg and Gla-300 provided similar reductions (p=0.370) in the rate of severe hypoglycaemia (Figure 3).9 Overall, results of the analysis showed that there was a similar reduction in HbA1c for patients switching to Gla-100, IDet and Gla-300, and similarly there was no significant difference between the second-generation treatments (Gla-300 and IDeg; p=0.591; Figure 4).9 Findings from this large, observational study of patients switching from any basal insulin to Gla-100, Gla-300, IDet or IDeg support the conclusions of DELIVER-D: that in real-world populations, second-generation basal insulin analogues provide similar efficacy and improved safety profiles versus first-generation agents. Both second-generation treatments (Gla-300 and IDeg) provided similar reductions in the rate of severe hypoglycaemia during a 6-month follow-up.
第二代基礎胰島素類似物
Second-generation Insulin Analogues – a Review of Recent Real-world Data and Forthcoming Head-to-head Comparisons

第二代胰島素類似物 Insulin Glargine 300U/mL簡稱 Gla-300, insulin degludec (簡稱IDeg-100)
Tresiba Insulin degludec U100
Tresiba Insulin degludec U100
第一代胰島素 insulin glargine 100U/mL 簡稱 Gla-100

IDeg-100 活性長達 42 小時, IDeg-100相較於 Gla-100 的降血糖能力, 可減少一天之內的血糖波動變化, 以及每天的血糖波動,
Gla-300 與 IDeg-100比較, 當給予每天每公斤 0.4 u 的劑量, 一天之內 Gla-300 的代謝活性變化比 IDeg-100減少 20%.
Second-generation basal insulin analogues (insulin glargine 300 U/mL [Gla-300; Sanofi, Paris, France] and insulin degludec [IDeg; Novo Nordisk, Bagsværd, Denmark]) have demonstrated similar efficacy in reducing HbA1c to first-generation insulin therapy (e.g. insulin glargine 100 U/mL [Gla-100; Sanofi]).18 However, the newer agents have longer and more stable pharmacokinetic (PK) and pharmacodynamic (PD) profiles than first-generation treatments.19–23 Gla-300 is associated with low within-day variability and high reproducibility (low betweenday variability) in insulin exposure,19,24 with predictable and stable glycaemic control well beyond 24 hours.25 Similarly, IDeg has demonstrated activity for up to 42 hours with four times lower day-to-day within-patient variability in glucose reduction compared with Gla-100.20 A comparison of the steady state PK/PD profiles of Gla300 and IDeg revealed that Gla-300 provided 20% less within-day fluctuation of metabolic activity than IDeg over 24 hours at a dose of 0.4 U/kg/day (Figure 1).
第二代胰島素類似物可達成與第一代胰島素 Gla-100相似的血糖控制效果, 但第二代胰島素的作用時間 > 24 小時, 血中藥物濃度可維持在較平穩的狀態, 因此可減少血糖波動, 注射時間也比較彈性化, 因此第二代基礎胰島素類似物適合做為一天一次的選擇
Second-generation basal insulin analogues (insulin glargine 300 U/mL [Gla-300; Sanofi, Paris, France] and insulin degludec [IDeg; Novo Nordisk, Bagsværd, Denmark]) have demonstrated similar efficacy in reducing HbA1c to first-generation insulin therapy (e.g. insulin glargine 100 U/mL [Gla-100; Sanofi]).18 However, the newer agents have longer and more stable pharmacokinetic (PK) and pharmacodynamic (PD) profiles than first-generation treatments.19–23 Gla-300 is associated with low within-day variability and high reproducibility (low betweenday variability) in insulin exposure,19,24 with predictable and stable glycaemic control well beyond 24 hours.25 Similarly, IDeg has demonstrated activity for up to 42 hours with four times lower day-to-day within-patient variability in glucose reduction compared with Gla-100.20 A comparison of the steady state PK/PD profiles of Gla300 and IDeg revealed that Gla-300 provided 20% less within-day fluctuation of metabolic activity than IDeg over 24 hours at a dose of 0.4 U/kg/day (Figure 1).
第二代胰島素類似物可達成與第一代胰島素 Gla-100相似的血糖控制效果, 但第二代胰島素的作用時間 > 24 小時, 血中藥物濃度可維持在較平穩的狀態, 因此可減少血糖波動, 注射時間也比較彈性化, 因此第二代基礎胰島素類似物適合做為一天一次的選擇
第二代胰島素類似物發生低血糖機率較低
在調整劑量的期間, Gla-300 造成的夜間低血糖機率較低
These advances have translated into the clinically meaningful benefit of providing similar glycaemic control to Gla-100, but with an ultra-long duration (>24-hour coverage), a more stable PK profile (resulting in reduced glycaemic variability), and greater injection time flexibility. These factors make second-generation basal insulin analogues suitable for once-daily treatment.19–23 In addition to effectively reducing HbA1c, the second-generation basal insulin analogues are associated with a lower risk of hypoglycaemia (both nocturnal hypoglycaemia and also, for Gla-300, all-day hypoglycaemia) compared with Gla-100 (Figure 2).18,27,28 For Gla-300, the benefit of lower incidence of hypoglycaemia is especially pronounced in the titration period.
結論
These advances have translated into the clinically meaningful benefit of providing similar glycaemic control to Gla-100, but with an ultra-long duration (>24-hour coverage), a more stable PK profile (resulting in reduced glycaemic variability), and greater injection time flexibility. These factors make second-generation basal insulin analogues suitable for once-daily treatment.19–23 In addition to effectively reducing HbA1c, the second-generation basal insulin analogues are associated with a lower risk of hypoglycaemia (both nocturnal hypoglycaemia and also, for Gla-300, all-day hypoglycaemia) compared with Gla-100 (Figure 2).18,27,28 For Gla-300, the benefit of lower incidence of hypoglycaemia is especially pronounced in the titration period.
結論
第二代基礎胰島素類似物可做為控制血糖的新療法, 第二代胰島素類似物降低 A1C 效果與第一代相似, 第二代基礎胰島素類似物還有其他臨床效益, 包括更穩定更長時間的作用, 一天施打一次即可. 任何時間都可以注射. 低血糖機率也降低.
Concluding remarks
The second-generation basal insulin analogues provide physicians with new treatment options for achieving targeted glycaemic control. While providing similar efficacy in lowering HbA1c to first-generation insulin analogues, the newer insulin treatment options provide additional clinical benefits, including a more stable, ultra-long duration of action that enables once-daily administration with flexibility in daily injection time, together with a lower risk of hypoglycaemia.
Concluding remarks
The second-generation basal insulin analogues provide physicians with new treatment options for achieving targeted glycaemic control. While providing similar efficacy in lowering HbA1c to first-generation insulin analogues, the newer insulin treatment options provide additional clinical benefits, including a more stable, ultra-long duration of action that enables once-daily administration with flexibility in daily injection time, together with a lower risk of hypoglycaemia.
第一代與第二代基礎胰島素類似物 Gla-300 vs IDeg-100 (degludec) vs 之間的比較
參考資料 Differentiating Basal Insulin Preparations: Understanding How They Work Explains Why They Are Different
第一代胰島素類似物
First-Generation Basal Insulin Analogs: Insulin Glargine 100 Units/mL and Insulin Detemir
第二代胰島素類似物
Second-Generation Basal Insulin Analogs: Insulin Glargine 300 Units/mL and Insulin Degludec 100 Units/mL and 200 Units/mL
第一代胰島素類似物
First-Generation Basal Insulin Analogs: Insulin Glargine 100 Units/mL and Insulin Detemir
第二代胰島素類似物
Second-Generation Basal Insulin Analogs: Insulin Glargine 300 Units/mL and Insulin Degludec 100 Units/mL and 200 Units/mL
第二代胰島素類似物明顯優於第一代
IDeg insulin degludec
IDet insulin detemir
Gla-100 insulin glargine 100 units/mL
Gla-300 insulin glargine 300 units/mL
將很多篇研究進行分析比較,
第一篇說 , 在T1DM病患, Gla-300 低劑量(0.4u/Kg)的藥效較穩定, 高劑量沒差異
但控糖效果比 IDeg-100 差, 低血糖機率高於 IDeg
第二第三篇研究提供的是間接比較
第四篇 DELIVER D+ study, 在 T2DM病患使用 Gla-300 與 IDeg-100, 比較後發現, 兩者控糖效果和低血糖機率相近
第五篇 LIGHTNING study發現, Gla-300 or IDeg 嚴重低血糖機率較 Gla-100 or IDet 低
第六篇 the CONFIRM real-world analysis發現, IDeg 優於 Gla-300, 低血糖較少, 控糖效果較好
第七篇The BRIGHT study發現, 在T2DM患者, 使用 Gla-300 的前期, 低血糖機率較 IDeg-100 低, 但最後兩者控糖效果相似, 整體低血糖機率相似,
Gla-300 比 IDeg-100, 低劑量使用時 (0.4u/kg/day)藥效更穩定, 分布較均勻, 但在較高劑量時沒有差異 (0.6u/kg/day).
從其他基礎胰島素換成 Gla-300 或 IDeg-100, 血糖控制結果相似, 低血糖發生率相似
CONFIRM real-world analysis 顯示, IDeg-100 與 Gla-300 比較, 血糖控制較佳, 低血糖機率較低, insulin retention 較佳. 但 real-world analysis 無法做到隨機分配, 仍需更多隨機研究證實
The BRIGHT study 比較 Gla-300 與 IDeg-100, 血糖控制結果相近, 整體低血糖機率相近, 但在研究開始的前一半時間內, 為降低血糖增加胰島素劑量時, Gla-300 低血糖機率較低
在調整胰島素劑量期間, Gla-300 發生低血糖的機率較 IDeg-100 低
Second-Generation Basal Insulin Analogs Compared with Each Other
The benefits of second-generation basal insulin analogs over first-generation are well established. Currently, comparison within class is clinically meaningful and such comparisons are emerging.
Gla-300 與 IDeg-100 比較
In a study that compared steady-state PK and PD profiles of Gla-300 and IDeg-100 in patients with T1D, Gla-300 provided a steadier PD profile (20% lower within-day fluctuation in GIR) and a more evenly distributed PK profile (Fig. 6) at a 0.4 units/kg/day dose; however, no significant differences were seen at the higher 0.6 units/kg/day dose [10].
A trial-level meta-analysis of the EDITION and BEGIN programs offered indirect comparison [45]. In the DELIVER D+ study, a direct comparison of real-world clinical outcomes with Gla-300 and IDeg showed that people with T2D switching from other basal insulins to two second-generation basal insulin analogs had comparable glycemic control, and incidence and rates of hypoglycemia [42].
Real-world analysis of electronic health records in the LIGHTNING study also demonstrated similar levels of glycemic control across basal insulins, but reported significantly lower rates of severe hypoglycemia in patients switching to Gla-300 or IDeg, compared with Gla-100 or IDet [46].
Among insulin-naïve patients with T2D, the CONFIRM real-world analysis showed that the group receiving IDeg had less hypoglycemia, greater glycemic control, and improved insulin retention compared with Gla-300 [47]. However, there are limitations to real-world observational analyses, with randomized controlled clinical trials needed to better understand differences between therapies.
The BRIGHT study is the first head-to-head randomized controlled trial comparing Gla-300 with IDeg in insulin-naïve patients with T2D. The study demonstrated comparable levels of glycemic control with similar overall incidence and rates of hypoglycemia. However, hypoglycemia was lower with Gla-300 during the first half of the study (titration period) when the greatest glucose reduction and insulin dose increase occurred.
Gla-100 insulin glargine 100 units/mL
Gla-300 insulin glargine 300 units/mL
將很多篇研究進行分析比較,
第一篇說 , 在T1DM病患, Gla-300 低劑量(0.4u/Kg)的藥效較穩定, 高劑量沒差異
但控糖效果比 IDeg-100 差, 低血糖機率高於 IDeg
第二第三篇研究提供的是間接比較
第四篇 DELIVER D+ study, 在 T2DM病患使用 Gla-300 與 IDeg-100, 比較後發現, 兩者控糖效果和低血糖機率相近
第五篇 LIGHTNING study發現, Gla-300 or IDeg 嚴重低血糖機率較 Gla-100 or IDet 低
第六篇 the CONFIRM real-world analysis發現, IDeg 優於 Gla-300, 低血糖較少, 控糖效果較好
第七篇The BRIGHT study發現, 在T2DM患者, 使用 Gla-300 的前期, 低血糖機率較 IDeg-100 低, 但最後兩者控糖效果相似, 整體低血糖機率相似,
Gla-300 比 IDeg-100, 低劑量使用時 (0.4u/kg/day)藥效更穩定, 分布較均勻, 但在較高劑量時沒有差異 (0.6u/kg/day).
從其他基礎胰島素換成 Gla-300 或 IDeg-100, 血糖控制結果相似, 低血糖發生率相似
CONFIRM real-world analysis 顯示, IDeg-100 與 Gla-300 比較, 血糖控制較佳, 低血糖機率較低, insulin retention 較佳. 但 real-world analysis 無法做到隨機分配, 仍需更多隨機研究證實
The BRIGHT study 比較 Gla-300 與 IDeg-100, 血糖控制結果相近, 整體低血糖機率相近, 但在研究開始的前一半時間內, 為降低血糖增加胰島素劑量時, Gla-300 低血糖機率較低
在調整胰島素劑量期間, Gla-300 發生低血糖的機率較 IDeg-100 低
Second-Generation Basal Insulin Analogs Compared with Each Other
The benefits of second-generation basal insulin analogs over first-generation are well established. Currently, comparison within class is clinically meaningful and such comparisons are emerging.
Gla-300 與 IDeg-100 比較
In a study that compared steady-state PK and PD profiles of Gla-300 and IDeg-100 in patients with T1D, Gla-300 provided a steadier PD profile (20% lower within-day fluctuation in GIR) and a more evenly distributed PK profile (Fig. 6) at a 0.4 units/kg/day dose; however, no significant differences were seen at the higher 0.6 units/kg/day dose [10].
A trial-level meta-analysis of the EDITION and BEGIN programs offered indirect comparison [45]. In the DELIVER D+ study, a direct comparison of real-world clinical outcomes with Gla-300 and IDeg showed that people with T2D switching from other basal insulins to two second-generation basal insulin analogs had comparable glycemic control, and incidence and rates of hypoglycemia [42].
Real-world analysis of electronic health records in the LIGHTNING study also demonstrated similar levels of glycemic control across basal insulins, but reported significantly lower rates of severe hypoglycemia in patients switching to Gla-300 or IDeg, compared with Gla-100 or IDet [46].
Among insulin-naïve patients with T2D, the CONFIRM real-world analysis showed that the group receiving IDeg had less hypoglycemia, greater glycemic control, and improved insulin retention compared with Gla-300 [47]. However, there are limitations to real-world observational analyses, with randomized controlled clinical trials needed to better understand differences between therapies.
The BRIGHT study is the first head-to-head randomized controlled trial comparing Gla-300 with IDeg in insulin-naïve patients with T2D. The study demonstrated comparable levels of glycemic control with similar overall incidence and rates of hypoglycemia. However, hypoglycemia was lower with Gla-300 during the first half of the study (titration period) when the greatest glucose reduction and insulin dose increase occurred.
基礎胰島素類似物 Tresiba Insulin degludec U100 第二代 長效
新一代超長效基礎胰島素Tresiba ®
第二代基礎宜島素類似物
(Insulin degludec U100; U200台灣未上市)
長效型基礎人類胰島素類似物,皮下注射。
Insulin degludec的生產流程是在酵母菌(Saccharomyces cerevisiae)中以重組去氧核醣核酸(DNA)表 現,接著進行化學修飾。
insulin degludec與人類 胰島素的差異在於缺少B30位置的胺基酸蘇胺酸 (threonine),並接上含麩胺酸(glutamic acid) 及C16脂肪酸的側鏈(化學名:LysB29 (Nεhexadecandioyl-γ-Glu) des (B30)人類胰島素)。
Tresiba® 注射到皮下組織後會形成多六聚體,產生 皮下insulin degludec團,從皮下組織吸收進入全 身循環的時間有延遲,較少一部分是由於 insulin degludec會與循環白蛋白結合。
半衰期約25小時, 有效作用時間可超過42小時。
研究顯示degludec U100與 glargine U100(第一代基礎宜島素類似物) 相比,作用時間更長、穩定性更好且沒有高峰期,不僅夜間低血糖發生率減少 25% [0.75 (0.58-0.97) 95% CI,P=0.026],更可顯著減少嚴重性低血糖症,且不會增加心血管疾病的風險。
第二代基礎宜島素類似物
(Insulin degludec U100; U200台灣未上市)
長效型基礎人類胰島素類似物,皮下注射。
Insulin degludec的生產流程是在酵母菌(Saccharomyces cerevisiae)中以重組去氧核醣核酸(DNA)表 現,接著進行化學修飾。
insulin degludec與人類 胰島素的差異在於缺少B30位置的胺基酸蘇胺酸 (threonine),並接上含麩胺酸(glutamic acid) 及C16脂肪酸的側鏈(化學名:LysB29 (Nεhexadecandioyl-γ-Glu) des (B30)人類胰島素)。
Tresiba® 注射到皮下組織後會形成多六聚體,產生 皮下insulin degludec團,從皮下組織吸收進入全 身循環的時間有延遲,較少一部分是由於 insulin degludec會與循環白蛋白結合。
半衰期約25小時, 有效作用時間可超過42小時。
研究顯示degludec U100與 glargine U100(第一代基礎宜島素類似物) 相比,作用時間更長、穩定性更好且沒有高峰期,不僅夜間低血糖發生率減少 25% [0.75 (0.58-0.97) 95% CI,P=0.026],更可顯著減少嚴重性低血糖症,且不會增加心血管疾病的風險。
甲狀腺亢進使用beta blocker約兩周(inderal/propranolol)
Beta blocker 乙型阻斷劑, 有不同劑型.
Inderal 10 mg 常使用於焦慮,緊張的病患
cordalol 40 mg.
作用
可以使交感神經興奮症狀改善。
具膜穩定(membrane stabilizing)作用的阻斷劑,如propranolol有少許抑制T4變成T3 的作用。
臨床上propranolol是最常用的藥 物,由於在甲狀腺機能亢進時,其代謝 速度會加速,所需劑量可能要較大
劑量
一般建議一天使用 80-160mg,分3-4次給予
例如 20 mg qid. 或 40 mg bid~qid
因作用機轉的關係,抗甲狀腺藥物會抑制甲狀腺中的濾泡釋放甲狀腺素,大約兩個禮拜之後原來在濾泡內之甲狀腺素便會釋放完畢,因此propranolol 使用約兩個禮拜後,如已無心悸、緊 張、手抖、怕熱等交感神經興奮的症狀 時即可停藥,不像抗甲狀腺藥物須長期使用。
(甲狀腺亢進服用procil 或 newmazole 至少需治療3周以上, 甲狀腺素才會降低, 通常是治療 6-8 周, 甲狀腺素才會降低)
另外. inderal 血中半衰期 3-6 小時. 最大濃度 peak 1~4 小時.
使用inderal 治療高血壓的維持劑量(120-240mg qd)會遠遠超過抗焦慮的劑量
Inderal 10 mg 常使用於焦慮,緊張的病患
cordalol 40 mg.
作用
可以使交感神經興奮症狀改善。
具膜穩定(membrane stabilizing)作用的阻斷劑,如propranolol有少許抑制T4變成T3 的作用。
臨床上propranolol是最常用的藥 物,由於在甲狀腺機能亢進時,其代謝 速度會加速,所需劑量可能要較大
劑量
一般建議一天使用 80-160mg,分3-4次給予
例如 20 mg qid. 或 40 mg bid~qid
因作用機轉的關係,抗甲狀腺藥物會抑制甲狀腺中的濾泡釋放甲狀腺素,大約兩個禮拜之後原來在濾泡內之甲狀腺素便會釋放完畢,因此propranolol 使用約兩個禮拜後,如已無心悸、緊 張、手抖、怕熱等交感神經興奮的症狀 時即可停藥,不像抗甲狀腺藥物須長期使用。
(甲狀腺亢進服用procil 或 newmazole 至少需治療3周以上, 甲狀腺素才會降低, 通常是治療 6-8 周, 甲狀腺素才會降低)
另外. inderal 血中半衰期 3-6 小時. 最大濃度 peak 1~4 小時.
使用inderal 治療高血壓的維持劑量(120-240mg qd)會遠遠超過抗焦慮的劑量
參考資料1 MayoClinic-Drugs and Supplements Propranolol (Oral Route)
For acute heart attack: For adrenal gland tumor (pheochromocytoma): For chest pain (angina): For high blood pressure (hypertension): For hypertrophic subaortic stenosis (thickened heart muscle): For irregular heartbeats: For migraine headaches: For proliferating infantile hemangioma: For tremors:
參考資料 2 應該是美國FDA的資料 Inderal®(propranolol hydrochloride)Tablets
DOSAGE AND ADMINISTRATION
- For oral dosage form (solution):
- Adults—180 to 240 milligrams (mg) per day, given in divided doses.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—At first, 40 milligrams (mg) three times a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—60 milligrams (mg) per day, given in divided doses for 3 days before having surgery. In patients who cannot have surgery, the usual dose is 30 mg per day, given in divided doses.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—60 milligrams (mg) per day, given in divided doses for 3 days before having surgery. In patients who cannot have surgery, the usual dose is 30 mg per day, given in divided doses.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (long-acting oral capsules):
- Adults—At first, 80 milligrams (mg) once a day. Your doctor may increase your dose as needed. The dose is usually not more than 320 mg per day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—80 to 320 milligrams (mg) per day, given in divided doses.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—80 to 320 milligrams (mg) per day, given in divided doses.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (extended-release capsules):
- Adults—At first, 80 milligrams (mg) once a day, given at bedtime. Your doctor may increase your dose as needed. However, the dose is usually not more than 120 mg per day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (long-acting oral capsules):
- Adults—At first, 80 milligrams (mg) once a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—At first, 40 milligrams (mg) two times a day. Your doctor may increase your dose as needed.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—At first, 40 milligrams (mg) two times a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (long-acting oral capsules):
- Adults—80 to 160 milligrams (mg) once a day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—20 to 40 milligrams (mg) three or four times a day, given before meals and at bedtime.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—20 to 40 milligrams (mg) three or four times a day, given before meals and at bedtime.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—10 to 30 milligrams (mg) three or four times a day, given before meals and at bedtime.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—10 to 30 milligrams (mg) three or four times a day, given before meals and at bedtime.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (long-acting oral capsules):
- Adults—At first, 80 milligrams (mg) once a day. Your doctor may increase your dose as needed. The dose is usually not more than 240 mg per day.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Adults—At first, 80 milligrams (mg) per day, given in divided doses. Your doctor may increase your dose as needed.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—At first, 80 milligrams (mg) per day, given in divided doses. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
- For oral dosage form (solution):
- Children 5 weeks to 5 months of age—Dose is based on your child's body weight and must be determined by the doctor. The starting dose is usually 0.6 milligram (mg) (0.15 milliliters [mL]) per kilogram (kg) of your child's body weight 2 times a day, taken at least 9 hours apart. Give the dose during or immediately after a feeding. Do not administer the dose if the infant is vomiting or not eating. After 1 week, the doctor will increase the dose to 1.1 mg (0.3 mL) per kg of body weight two times a day. After 2 weeks, the doctor will increase the dose to 1.7 mg (0.4 mL) per kg of body weight 2 times a day, taken for 6 months.
- Children under 5 weeks of age—Use is not recommended.
- For oral dosage form (solution):
- Adults—At first, 40 milligrams (mg) two times a day. Your doctor may increase your dose as needed.
- Children—Dose is based on body weight and must be determined by your doctor.
- For oral dosage form (tablets):
- Adults—At first, 40 milligrams (mg) two times a day. Your doctor may increase your dose as needed.
- Children—Use and dose must be determined by your doctor.
DOSAGE AND ADMINISTRATION
General Because of the variable bioavailability of propranolol, the dose should be individualized based on response.
Hypertension
The usual initial dosage is 40 mg Inderal twice daily, whether used alone or added to a diuretic. Dosage may be increased gradually until adequate blood pressure control is achieved. The usual maintenance dosage is 120 mg to 240 mg per day. In some instances a dosage of 640 mg a day may be required. The time needed for full antihypertensive response to a given dosage is variable and may range from a few days to several weeks. While twice-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, some patients, especially when lower doses are used, may experience a modest rise in blood pressure toward the end of the 12-hour dosing interval. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. If control is not adequate, a larger dose, or 3-times-daily therapy may achieve better control.
Angina Pectoris
Total daily doses of 80 mg to 320 mg Inderal, when administered orally, twice a day, three times a day, or four times a day, have been shown to increase exercise tolerance and to reduce ischemic changes in the ECG. If treatment is to be discontinued, reduce dosage gradually over a period of several weeks. (See WARNINGS.)
Atrial Fibrillation
The recommended dose is 10 mg to 30 mg Inderal three or four times daily before meals and at bedtime.
Hypertension
The usual initial dosage is 40 mg Inderal twice daily, whether used alone or added to a diuretic. Dosage may be increased gradually until adequate blood pressure control is achieved. The usual maintenance dosage is 120 mg to 240 mg per day. In some instances a dosage of 640 mg a day may be required. The time needed for full antihypertensive response to a given dosage is variable and may range from a few days to several weeks. While twice-daily dosing is effective and can maintain a reduction in blood pressure throughout the day, some patients, especially when lower doses are used, may experience a modest rise in blood pressure toward the end of the 12-hour dosing interval. This can be evaluated by measuring blood pressure near the end of the dosing interval to determine whether satisfactory control is being maintained throughout the day. If control is not adequate, a larger dose, or 3-times-daily therapy may achieve better control.
Angina Pectoris
Total daily doses of 80 mg to 320 mg Inderal, when administered orally, twice a day, three times a day, or four times a day, have been shown to increase exercise tolerance and to reduce ischemic changes in the ECG. If treatment is to be discontinued, reduce dosage gradually over a period of several weeks. (See WARNINGS.)
Atrial Fibrillation
The recommended dose is 10 mg to 30 mg Inderal three or four times daily before meals and at bedtime.
2020 糖尿病血糖控制 第二型糖尿病的藥物治療建議
PHARMACOLOGIC THERAPY FOR TYPE 2 DIABETES
Recommendations
第二型糖尿病建議使用 metformin 作為起始治療
9.4 Metformin is the preferred initial pharmacologic agent for the treatment of type 2 diabetes. A
開始治療後, 應持續使用 metformin , 除非病患無法忍受副作用, 或有禁忌症, 其他抗糖尿病藥物, 包括胰島素, 可以與 metformin 合併使用
9.5 Once initiated, metformin should be continued as long as it is tolerated and not contraindicated; other agents, including insulin, should be added to metformin. A
有些病患在剛開始治療的時候, 可以早期使用組合式療法, 可以延緩治療失敗
9.6 Early combination therapy can be considered in some patients at treatment initiation to extend the time to treatment failure. A
有些狀況應早點使用胰島素: 有代謝症狀 (體重減輕), 有高血糖症狀, A1C > 10%, 血糖 > 300,
9.7 The early introduction of insulin should be considered if there is evidence of ongoing catabolism (weight loss), if symptoms of hyperglycemia are present, or when A1C levels (>10% [86 mmol/mol]) or blood glucose levels (≥300 mg/dL [16.7 mmol/L]) are very high. E
應以病患為中心選擇藥物, 考量心血管疾病, 低血糖風險, 體重, 費用, 發生副作用機率, 以及病患選擇
9.8 A patient-centered approach should be used to guide the choice of pharmacologic agents. Considerations include cardiovascular comorbidities, hypoglycemia risk, impact on weight, cost, risk for side effects, and patient preferences (Table 9.2 and Figure 9.1). E
糖尿病患, 如果已有動脈粥狀硬化, 或是動脈粥狀硬化風險高, 或心臟衰竭, 可考慮使用 SGLT2i 或 GLP1RA, 這兩類藥物有助於心血管疾病, 對於心血管疾病益處與 A1C 數值無關.
9.9 Among patients with type 2 diabetes who have established atherosclerotic cardiovascular disease or indicators of high risk, established kidney disease, or heart failure, a sodium–glucose cotransporter 2 inhibitor or glucagon-like peptide 1 receptor agonist with demonstrated cardiovascular disease benefit (Table 9.1, Table 10.3B, Table 10.3C) is recommended as part of the glucose-lowering regimen independent of A1C and in consideration of patient-specific factors (Figure 9.1). A
第二型糖尿病如需大幅度降低血糖, 使用口服藥物無法達到血糖治療目標, 可考慮使用 GLP1RA, 優先順位在胰島素之前.
9.10 In patients with type 2 diabetes who need greater glucose lowering than can be obtained with oral agents, glucagon-like peptide 1 receptor agonists are preferred to insulin when possible. B
第二型糖尿病如果血糖無法達到治療目標, 需即早考慮合併其他藥物治療
9.11 Intensification of treatment for patients with type 2 diabetes not meeting treatment goals should not be delayed. B
每 3-6 個月需重新評估藥物組合及服藥習慣, 將會影響治療的其他因素列入考量
9.12 The medication regimen and medication-taking behavior should be reevaluated at regular intervals (every 3–6 months) and adjusted as needed to incorporate specific factors that impact choice of treatment (Fig. 4.1 and Table 9.1). E
第十二章 老年人的血糖控制目標 Recommendations
如果過去健康, 沒有其他慢性疾病, 認知功能正常, 日常生活功能正常, 控制 A1C < 7.5%
如果有多重慢性共病症, 認知功能障礙, 功能異常, 血糖控制目標可以較寬鬆, A1C < 8.0-8.5%
12.5 Older adults who are otherwise healthy with few coexisting chronic illnesses and intact cognitive function and functional status should have lower glycemic goals (such as A1C <7.5% [58 mmol/mol]), while those with multiple coexisting chronic illnesses, cognitive impairment, or functional dependence should have less-stringent glycemic goals (such as A1C <8.0–8.5% [64–69 mmol/mol]). C
老人的血糖控制目標可以稍微寬鬆, 但應避免高血糖引起症狀, 或急性高血糖併發症風險,
12.6 Glycemic goals for some older adults might reasonably be relaxed as part of individualized care, but hyperglycemia leading to symptoms or risk of acute hyperglycemia complications should be avoided in all patients. C
老年人的糖尿病併發症篩檢應客製化, 多注意可能會導致功能異常的併發症
12.7 Screening for diabetes complications should be individualized in older adults. Particular attention should be paid to complications that would lead to functional impairment. C
高血壓治療目標應根據每個病患訂定各別目標
12.8 Treatment of hypertension to individualized target levels is indicated in most older adults. C
治療其他心血管疾病危險因子, 對於老人應客製化, 考量其預期壽命, 視情況給予降血脂治療及aspirin 治療.
12.9 Treatment of other cardiovascular risk factors should be individualized in older adults considering the time frame of benefit. Lipid-lowering therapy and aspirin therapy may benefit those with life expectancies at least equal to the time frame of primary prevention or secondary intervention trials. E
12.9 Treatment of other cardiovascular risk factors should be individualized in older adults considering the time frame of benefit. Lipid-lowering therapy and aspirin therapy may benefit those with life expectancies at least equal to the time frame of primary prevention or secondary intervention trials. E
基礎胰島素 NPH 與 基礎宜島素類似物 basal insulin analogue
口服藥治療無法達標時,GLP1受體促效劑優於胰島素使用
名詞定義:
名詞定義:
2001年,研究者提出了「 臨床惰性(clinical inertia)」的概念, 意思是發現問題之後沒有做改善.
treatment inertia 治療慣性, 治療惰性, A1C 未達治療目標, 卻不改變治療策略, 醫病雙方沒有積極使用胰島素
Therapeutic Inertia 同上。
用來作為基礎胰島素的有中效胰島素NPH insulin與長效型胰島素類似物
長效胰島素類似物包括: insulin glargine (Lantus®)及insulin detemir(Levemir®)
NPH 在1940年代開始使用
第一代基礎胰島素於 2000年上市
第二代基礎胰島素於 2015年上市
Human Basal Insulin: NPH Insulin
First-Generation Basal Insulin Analogs: Insulin Glargine 100 Units/mL(簡稱Gla-100) and Insulin Detemir *(簡稱IDet)新一代的胰島素筆, 可以一次施打 160u 的 Gla-300 or IDeg-200. 好處是可以減少施打次數, 可以降低胰島素筆的數量 (台灣只有 IDeg-100)
a once-daily dose can be administered using a pen device that can deliver up to 160 units of Gla-300 or IDeg-200. This larger delivery dose reduces the number of injections and the number of pens required.
Gla-100 第一代基礎胰島素類似物
IDet 第一代基礎胰島素類似物
Gla-300 第二代基礎胰島素類似物
(IDeg-100) 第二第基礎胰島素類似物
Gla-300 相較於 Gla-100, 降血糖效果較穩定, 血中藥物濃度較穩定 (distributed PK/PD profiles), 濃度減低的時間較長 (50% of the area under the serum insulin)
使用連續性血糖監測, glycemic excursions Gla-300 早上或晚上施打結果相似, 但早上施打 Gla-100 會有較高的血糖上升
Gla-300 相較於 Gla-100, 血糖控制效果相近, 但嚴重低血糖及夜間低血糖機率較低
不過也有研究顯示, Gla-300 與 Gla-100 的低血糖機率差異不大.
RESULTS:
At steady state, insulin concentration (INS) and glucose infusion rate (GIR) profiles of Gla-300 were more constant and more evenly distributed over 24 h compared with those of Gla-100 and lasted longer, as supported by the later time (∼ 3 h) to 50% of the area under the serum INS and GIR time curves from time zero to 36 h post dosing. Tight blood glucose control (≤ 105 mg · dL(-1)) was maintained for approximately 5 h longer (median of 30 h) with Gla-300 compared with Gla-100.
另一篇研究發現, 第一型糖尿病患, 發生低血糖的事件, Gla-100組每人每年 9次, Gla-300 每人每年 4次.
A randomized controlled study in people with T1D using continuous glucose monitoring also found that nocturnal confirmed and severe hypoglycemia rates were lower with Gla-300 than with Gla-100 (4.0 versus 9.0 events per participant-year)
(下面是第一代與第二代比較) IDeg-100 相較於 Gla-100, 低血糖機率降低 21%, 夜間低血糖機率降低 52%,
另一篇研究發現, IDeg-100 相較於 Gla-100 可將低血糖機率降低 11%-30%.
DEVOTE研究: 第二型糖尿病患使用 IDeg-100 可顯著降低嚴重低血糖發生率(4.9% vs 6.6%)
In the SWITCH 1 and 2 clinical trials, people with T1D or type 2 diabetes (T2D) treated with IDeg had reduced rates of overall symptomatic hypoglycemia compared with those treated with Gla-100 (SWITCH 1, risk ratio 0.89; SWITCH 2, risk ratio 0.70) [35, 36]. In the DEVOTE study, participants with T2D receiving IDeg had significantly lower rates of severe hypoglycemia compared with those receiving Gla-100 (4.9% vs. 6.6%, respectively; rate ratio 0.60)
研究發現, 使用 Gla-300 發生低血糖的機率較 Gla-100 或 IDet 低 (相較機率 0.75 及 0.43)
In the DELIVER 2 and 3 studies, significantly fewer patients treated with Gla-300 experienced hypoglycemia compared with Gla-100 or IDet (adjusted odds ratio 0.75 and 0.43, respectively).
Gla-300 用量比 Gla-100 需增加 10-20%, 使用 Gla-100 的病患如果要改用 Gla-300 需注意換算劑量. 不過這種換算比例並非絕對, 也可能與病患本身有關.
使用Gla-300與其他基礎胰島素比較, 在相近的劑量下, Gla-300血糖控制( glycated hemoglobin targets )較好, 且低血糖機率較低.
參考資料 內科學誌 2010 長效型胰島素類似物在第2型糖尿病人的應用(馬偕內分泌暨新陳代謝科)
基礎胰島素使用時機: 第二型糖尿病, 若使用 一種或兩種口服降血糖藥物治療後,而 A1C 仍≧7%,就應考慮加上基礎胰島素
基礎胰島素使用方式:
~ 睡前打一次insulin glargine或insulin detemir 或是NPH
~ insulin glargine或insulin detemir也可以選擇早上注射。
起始劑量: (口服抗糖尿病藥物續用)
每天 10u, 或每公斤 0.2u.
如果病患血糖很高, 起始劑量可以提高到每天 20u.
每天測血糖, 如果血糖仍未到達目標, 每三天增加 2u.
如果血糖超過 180 可以加大增幅, 例如每三天增加 4u.
空腹血糖目標範圍(70-130 mg/dL) 新的文章說 80-130 mg/dL
ADA與EASD建議患者注射基礎胰島素後空腹血糖的目標訂為≦130 mg/dL
但很多研究則將目標訂在 120 甚至 100 以下
若患者低血糖風險低, 建議將目標訂嚴格一點 (100 或 120 以下)
飯後血糖標準 (80-160) 較寬鬆一點.
飯後血糖標準 (80-160) 較寬鬆一點.
如果空腹血糖達標, 但 A1C 仍高, 需測量每餐之前的血糖及睡前血糖
飯前血糖最高的那一次, 可餐前追加第二次注射速效胰島素,
追加注射速效胰島素的起始劑量 4u. 之後每三天可增加2u. 直到血糖達標
如果再追蹤三個月 A1C 仍高. 可以追加第三次餐前速效胰島素注射.
如果再追蹤三個月 A1C 仍未達標, 可測量飯後血糖, 依照飯後血糖調整餐前速效胰島素注射量.
biphasic insulin/prandial insulin
有一篇研究, 比較加上每日兩次biphasic insulin (insulin aspart 30 短效)、每日三次prandial insulin (insulin aspart 短效) 及每日一次或兩次basal insulin (insulin detemir長效)的效果。
治療一年後糖化血色素分別下降1.3%、1.4%與0.8%,糖化血色素≦6.5%的比率分別為17.0%、23.9%與8.1%,統計上biphasic insulin與 prandial insulin兩組沒有差別但皆比basal insulin組要好。
第一年糖化血色素連續兩次≧8.0%或第二年糖化血色素仍>6.5%的患者,則停用sulfonylurea加上第二種胰島素
biphasic insulin組~~ 中餐多注射prandial insulin一次
prandial insulin組~~ 睡前加上basal insulin
basal insulin組~~ 三餐分別加上prandial insulin
治療三年後biphasic insulin組、prandial insulin組與basal insulin組分別有67.7%、73.6%及81.6%的患者使用第二種胰島素,糖化血色素比尚未使用胰島素前分別下降1.3%、1.4%與1.2%,統計上三組間沒有差異。
糖化血色素≦6.5%的比率在prandial insulin組(44.79%)與basal insulin組(43.2%)皆比biphasic insulin組(31.9%)要高發生低血糖的中位數以prandial insulin組(5.7/patient/year)最高、biphasic insulin組(3.0/patient/year)次之,basal insulin組(1.7/patient/year)最低。
體重增加方面,basal insulin組(3.6 kg)比prandial insulin組(6.4 kg)及biphasic insulin組(5.7 kg)都要少。
其中以basal insulin為基礎的治療,發生低血糖的機會與體重的增加都最低
biphasic, 糖化血色素≦6.5%比率(勝), 低血糖機率(中), 體重增加 (中)
臨床上使用基礎胰島素, 加上速效胰島素的方式
-- 主要一餐前, 打速效胰島素
-- 使用預混型胰島素(如NovoMix® 30, (lispromix 50/50), 早晚各打一次
-- 三餐前打速效胰島素, 降血糖效果比預混BID好.
參考資料 injected insulin
基礎胰島素 basal insulin 一天注射一至兩次, 維持整天的穩定胰島素濃度, 讓血糖保持在穩定值, 但僅使用 basal insulin 無法涵蓋用餐後的血糖上升.
餐後血糖 prandial insulins 在用餐之後使用, 作用快速, 降低餐後血糖
Basal vs. Prandial: Insulins can be divided into two categories based on function: basal (long-acting insulin) and prandial (rapid-acting or “mealtime” insulin). Basal insulin is designed to be injected once or twice daily to provide a constant level of insulin action throughout the day. Basal insulin helps keep blood sugars at a consistent level when you are not eating, but it is not enough to cover glucose spikes after mealtime. Prandial insulins, on the other hand, are taken at mealtime and act rapidly on the body, serving to bring down the high sugar levels following meals.
胰島素的結構可分兩類, 人類胰島素及胰島素類似物. 胰島素類似物的價格較高, 但能避免低血糖與體重增加. 整體醫療費用(低血糖掛急診,住院)也許可以降低
Analog vs. Human Insulin: There are also two types of insulin structures: human insulin and analog insulin. Human insulins were developed first and are essentially identical in structure to the insulin produced in the body. Analog insulins are similar in structure but have minor biological modifications to give them desirable properties. While analog insulins cost more, they generally lead to less hypoglycemia and weight gain. Prandial (mealtime) insulin analogs tend to act faster than human insulin.
參考資料 First Online: 30 March 2019
prandial insulins 作用快, 降低餐後血糖
basal insulins 作用時間長, 改善 24 小時血糖控制
clinical action profiles 臨床作用輪廓
研究證實, 第二代基礎胰島素類似物, insulin glargine U300 及 insulin degludec U100 U200, 一天施打一次, 能提供穩定的血糖控制, 且可降低低血糖機率 (相較於第一代的 insulin glargine U100 及 insulin detemir), 所以可以減少病患整體醫療花費(去醫院的機率)
Insulin glargine 及 insulin detemir 與 NPH的比較
NPH造成夜間低血糖的機率較高(半夜三點測血糖)
注射insulin detemir比注射insulin glargine的患者體重增加較少
參考資料~糖尿病筆記
基礎胰島素包括了
舊的人類胰島素(NPH)
長效胰島素類似物(Insulin Glargine U-100以及Insulin Levemir)
更長效胰島素類似物(Insulin Glargine U-300以及Insulin Degludec)
台灣目前核准使用的基礎胰島素
第二代基礎胰島素: Insulin glargine U-300 及 Insulin Degludec Detemir,Insulin Glargine U-100
GLP1RA 健保給付規定:
Liraglutide(如 Victoza): 當患者已接受口服降血糖藥物,及/或基礎胰島素治療仍未達理想血糖控制時,與口服降血糖藥物及/或基礎胰島素併用。本藥品不得與 DPP-4抑制劑、SGLT-2抑制劑併用。
而 Exenatide(如 Byetta)、dulaglutide(如 Trulicity) 仍規定不可以與基礎胰島素併用
基礎胰島素與GLP1RA合併的藥物:
Xultophy, 組成每1毫升(mL)含有 100單位的 Degludec 與 3.6mg 的 Liraglutide
隨餐胰島素 aspart 三餐給予, 起始劑量, 0.1U/公斤
使用基礎胰島素達到空腹血糖穩定或是每日每公斤0.5單位以上, 但 HbA1C 糖化血色素尚未達標,考慮合併注射治療
-- 基礎胰島素加上GLP1受體促效劑 (較不會低血糖也比較不會體重增加。)
-- 一天多次胰島素注射。
使用胰島素治療後
-- 病患需自己監控血糖
-- 可維持使用Metformin。
-- SU和DPP4抑制劑考慮停用
-- 如果使用到大劑量胰島素,可考慮續用TZD或是SGLT2抑制劑來降低胰島素劑量
from uptodate Choice of basal insulin 基礎胰島素的選擇
insulin NPH or detemir given at bedtime
insulin glargine or degludec given in the morning or bedtime
每天注射一次胰島素, 可選擇睡前打 NPH or Detemir , 或者每天早上/睡前, 打一次 insulin glargine or degludec.
有些國家的 NPL 製作成單一劑型, 但在美國, NPL 僅有與速效胰島素 lispro 搭配的組合劑型.
A single daily dose of either insulin NPH or detemir given at bedtime or insulin glargine or degludec given in the morning or at bedtime is a reasonable initial regimen (table 1). In practice, payer coverage is often an important consideration in the selection of basal insulin. In some countries, NPL is available as a separate insulin analog for basal coverage [22,23]. In the United States, NPL is only available in combination with rapid-acting lispro (insulin lispro protamine-insulin lispro).
不同的基礎胰島素對於血糖控制差異不大, 在胰島素類似物中, insulin glargine, Detemir, degludec 這三種藥物比起 NPH, 較少造成夜間低血糖, 但缺點是價格較貴. 使用這些藥物造成低血糖需住院或需掛急診的機率並無差異
The basal insulin preparations do not differ significantly in glycemic efficacy [24,25]. Among basal insulin preparations, insulin glargine, detemir, and degludec may have less nocturnal hypoglycemia (but not always total hypoglycemia) compared with NPH, with the important disadvantage of high cost. There does not appear to be any difference in hypoglycemia-related hospital admissions or emergency department visits. As examples:
將研究資料做統合分析, 比較每天打一次 insulin glargine or detemir, 與每天 1-2 次打 NPH, 所有基礎胰島素改善A1c的結果相似, 但有些統合分析發現, 使用 insulin glargine or detemir 的這組, 有症狀及夜間低血糖的機率比使用NPH的這組低, 不過基礎胰島素造成低血糖的機率原本就不是很高.
●In meta-analyses of trials comparing once-daily insulin glargine or detemir with once-daily or twice-daily NPH insulin, there were similar improvements in A1C with all types of basal insulin [25-28]. However, in some of the meta-analyses, the rates of overall symptomatic and nocturnal hypoglycemia (while relatively infrequent with either basal insulin) were lower in patients treated with either insulin glargine or detemir compared with NPH [25-27].
一篇回溯性觀察性研究發現, 使用 insulin analogs 與 NPH比較, 並不會降低掛急診或住院的低血糖事件, 但NPH這組的血糖控制稍微好些(8.2 VS 7.9 )
●In a retrospective observational study using data from a large health care delivery system (>25,000 patients initiating basal insulin), there was no benefit of insulin analogs compared with NPH in reducing emergency department or hospital admissions for hypoglycemia (11.9 versus 8.8 events per 1000 person-years, respectively) despite slightly better glycemic control in the NPH group (achieved A1C 8.2 versus 7.9 percent with NPH, suggesting they were not treated with less aggressive doses) [29].
Insulin degludec (IDeg-100) 降血糖效果與 insulin glargine (Gla-100)相似, 有些研究發現 insulin degludec (IDeg-100) 的低血糖機率較低, 尤其是對於採嚴格血糖控制的病患在一個雙盲世代研究, 經 65周的追蹤, 共收錄第二型糖尿病患者 721 位, 平均A1C 7.6, 且病患至少有一個低血糖的危險因子, 隨機分配至 一天打一次 insulin degludec (IDeg-100) 或 insulin glargine(Gla-100) , 治療 32 周後, 換成其他替代胰島素, 再繼續治療 32 周, 所有低血糖及夜間低血糖事件, 在 degludec 這組較低, 但發生嚴重低血糖的機率則無差異. 兩組的血糖控制相似
基礎胰島素IDeg-100與Gla-100低血糖機率比較
基礎胰島素IDeg-100與Gla-100低血糖機率比較
Insulin degludec appears to have similar glycemic efficacy as that of insulin glargine and, in some trials, a lower rate of hypoglycemia, especially if aiming for more stringent glycemic targets [17,30-33]. As an example, in a 65-week, double-blind, crossover trial, 721 adults with type 2 diabetes (mean A1C 7.6 percent) and at least one risk factor for hypoglycemia were randomly assigned to receive once-daily insulin degludec or insulin glargine for 32 weeks and then crossed over to the alternate insulin treatment for the next 32 weeks [34]. The rate of overall (185.6 versus 265.4 episodes per 100 patient-years of exposure) and nocturnal (55.2 versus 93.6 episodes) symptomatic hypoglycemia was lower with degludec (rate ratios 0.70, 95% CI 0.61-0.80 and 0.58, 95% CI 0.46-0.74, respectively). There was no difference in relatively rare severe hypoglycemia (nonsignificant reduction of 0.62 episodes per 100 patient-years with degludec). Overall glycemic control was similar (A1C 7 to 7.1 percent).
雖然 degludec (IDeg-100) 顯著降低整體低血糖與夜間低血糖機率(平均每五年減少一次事件), 但還要考量最大效益與花費是否值得, 而 insulin degludec (IDeg-100) 長期的安全性尚未得知
Although degludec significantly reduced overall and nocturnal hypoglycemia, the modest benefit (on average, one episode less every five years) must be balanced against its relatively higher cost. In addition, the long-term safety profile of insulin degludec is unknown [35].
訂閱:
文章 (Atom)
麻疹與麻疹疫苗.MMR疫苗
2025-10-03 09:30AM 之前國內出現麻疹疫情時. 有部分醫護人員需施打麻疹疫苗. 建議接種的族群. 最初是1981年之後出生補接種一劑. 後來修訂為1966年之後出生補接種一劑 不具免疫力的醫療人員補接種兩劑(間隔至少四周) 114-01-10 疾病管制署致醫界通函...
-
【登山醫學】虎頭蜂-賴育民醫師-發表於2014/08/25 山野活動中,該如何避免遭遇這些惱人的虎頭蜂呢? 認識虎頭蜂 虎頭蜂並不是單一的蜂種,而是泛指胡蜂科的大型蜂類,在台灣一共有七種,也有人稱之為大黃蜂。胡蜂科的成員是肉食性的,但也攝食花蜜和水果,體型碩大,毒性和攻擊性都比蜜...
-
2025-01-20 中午 12:34 剛剛查詢 secorine 成分. 其中有一種是甲基麻黃素. 之前看過報導說. 含有甲基麻黃素的藥物被美國FDA禁用. 所以查了一下相關報導 常見的麻黃素類的藥物有三種(注意它們中間的字母有點不同: ephed 與 eph) 1. 甲基麻黃...
-
腎衰竭可以用, 不用調整劑量, 可與胰島素並用 劑量: 一般人 5mg QD. 可做為單一藥物治療糖尿病 可與其他藥物併用 肝功能不良不用調整劑量 *(肝腎不全無需調整劑量) 老年人無需調整劑量 服用方式 可 隨餐 服用或 空腹 服用, 食物不影響吸收 與胰島...







